CRISPR gene editing has revolutionized the landscape of modern biology, introducing unprecedented capabilities for addressing genetic disorders. This cutting-edge gene editing technology holds the promise of curing ailments like sickle cell anemia by allowing scientists to precisely alter genes at the molecular level. However, the rise of CRISPR also raises significant CRISPR ethics questions as advancements confront society with a complex web of moral implications. As we explore the potential for health equity in accessing these innovative solutions, we must consider who benefits from such breakthroughs in gene editing technology. Balancing the allure of a cure with the ethical dilemmas it presents is essential for forging a responsible path forward in genetic research and application.
The genetic modification landscape has been dramatically altered by recent advancements in gene editing tools, particularly CRISPR technology. This innovative approach, which allows for targeted alterations in DNA sequences, opens the door to potential medical breakthroughs, including the treatment of genetic diseases like sickle cell anemia. However, alongside these developments arise pressing bioethics concerns, as society wrestles with the implications of modifying human genetics. Ensuring that advancements contribute to health equity is vital, as access to such technological innovations may be unevenly distributed. As we navigate the implications of gene transformation, the question lingers: how do we balance scientific progress with ethical considerations?
Understanding CRISPR Gene Editing Technology
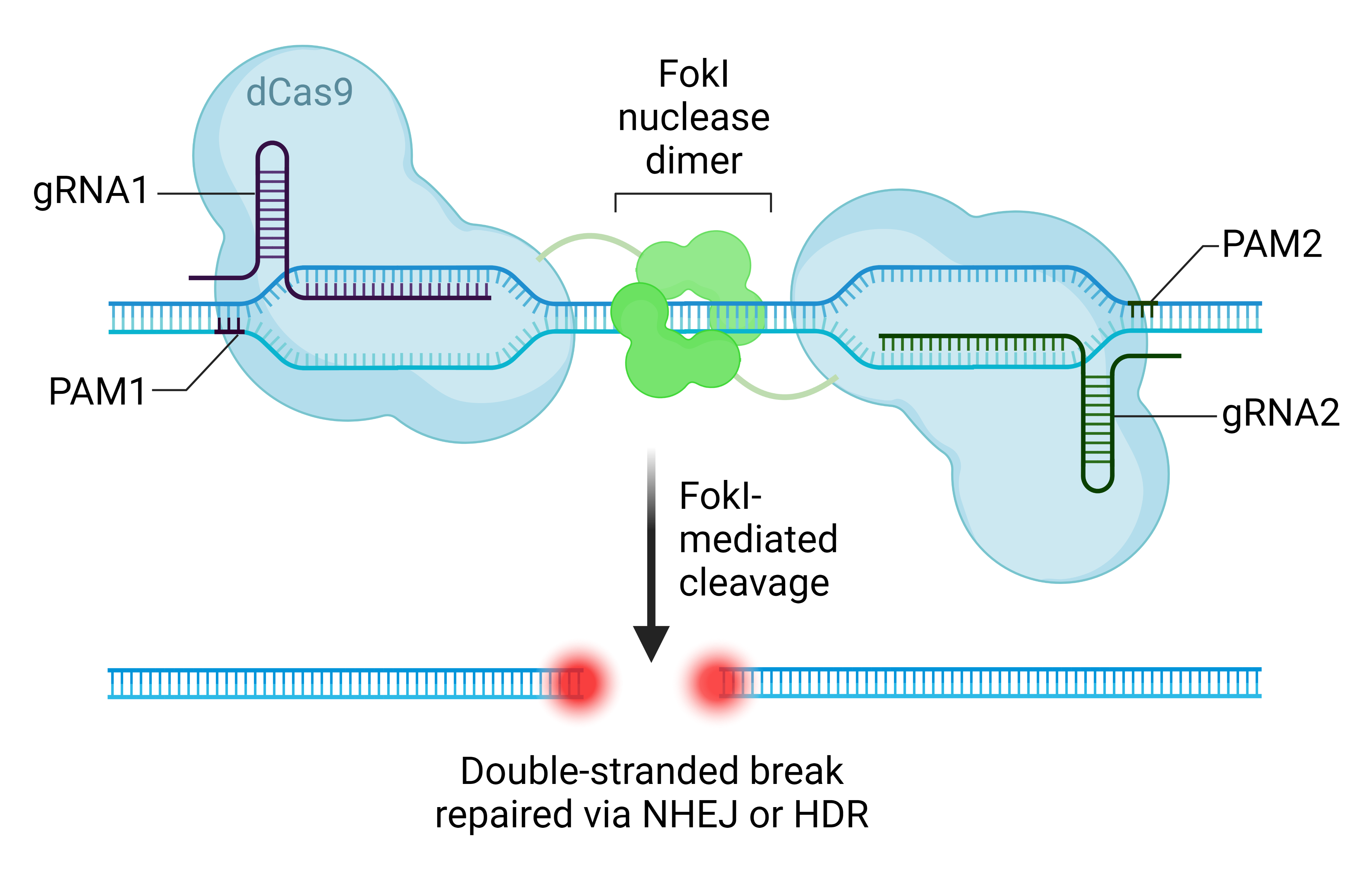
CRISPR gene editing technology represents a groundbreaking advancement in the field of genetics and molecular biology. By utilizing a naturally occurring mechanism found in bacteria, scientists can now accurately edit specific sequences of DNA. This precise editing capability allows for the alteration of genetic information in organisms, potentially addressing a variety of genetic disorders and diseases. The excitement surrounding CRISPR is primarily due to its efficacy and efficiency, making it easier than ever to envision cures for conditions such as sickle cell anemia.
Moreover, CRISPR’s ability to work on both somatic and germline cells opens a multitude of possibilities for future applications. Somatic gene editing, which affects only the individual without altering their genetic makeup passed to offspring, could mean the eradication of sickle cell disease within patients. On the other hand, germline editing offers the prospect of preventing hereditary conditions from being passed on to future generations, raising both hopeful expectations and ethical dilemmas that society must navigate.
The Ethical Considerations of Gene Editing
As discussions surrounding CRISPR technology advance, so too must our contemplation of the ethical implications involved. The potential to edit genes leads to crucial questions: should we intervene in the genetic makeup of future generations? Who decides what traits are desirable, and how do we ensure equitable access to such transformative treatments? The ethical considerations surrounding CRISPR gene editing are not just theoretical; they encompass real societal concerns about health equity and the ramifications of creating a ‘designer baby’ culture.
Bioethicists like Rebecca Weintraub Brendel emphasize the importance of examining these ethical issues rigorously. Discussions about gene editing should not only focus on what is possible but also on what is right and fair. The realities of health equity come into play when considering the staggering costs of treatments made possible by CRISPR. With therapies like the sickle cell cure priced around $2.2 million, it is imperative that we address who will benefit from these advancements and ensure such innovations do not widen the existing health disparities.
Curing Sickle Cell Disease: A Double-Edged Sword
The promise of CRISPR in curing sickle cell disease has ignited hope among patients and healthcare providers alike. By targeting the mutations in hemoglobin genes, scientists can effectively mitigate the symptoms and complications associated with this debilitating condition. The prospect of relief for the approximately 100,000 Americans suffering from sickle cell highlights the transformative potential of gene editing technology. However, this promise must be weighed against significant ethical concerns, including access and long-term consequences.
Despite its potential benefits, the offer of a ‘cure’ raises questions surrounding consent and the rights of patients. Should parents decide the genetic attributes of their children, especially in cases where the disease is manageable? As Neal Baer and others discuss, these dilemmas are not easily answered. The implications extend beyond individual cases and touch on broader societal issues, compelling us to confront uncomfortable truths about our values and priorities when it comes to healthcare.
Health Equity: Addressing Disparities in Gene Editing Access
Health equity stands as a cornerstone of the conversation about CRISPR gene editing. As the technology progresses, it becomes crucial to ensure that all populations, particularly those historically marginalized, have access to transformative genetic therapies. The disparity in access to healthcare resources raises pressing questions about who benefits from advancements in gene editing technology and who is left behind. Without intentional policy interventions, CRISPR could potentially exacerbate existing health inequalities.
As experts like Brendel point out, innovation in medicine often produces unequal benefits, heightening the philosophical and practical debates about fairness in healthcare. The responsibility falls upon policymakers, healthcare providers, and society at large to craft solutions that ensure equitable access to CRISPR therapies. This will require a concerted effort to address economic barriers and guarantee that gene editing technologies are not simply privileges for the affluent, but accessible solutions for all.
Navigating the Regulations of Gene Editing
As the potential of CRISPR gene editing technology unfolds, so does the need for comprehensive regulations that address its ethical implications. Currently, the landscape of gene editing legislation varies widely across different countries, with some regions like the U.S. exhibiting strict restrictions on germline editing while others remain more permissive. This regulatory landscape places significant emphasis on ensuring that gene editing technology is utilized ethically and safely, protecting individuals and society from potential abuses.
Moreover, the international dimension of gene editing oversight raises questions about accountability and monitoring. With advances being made around the world, including in countries where regulations may be looser, the need for a coordinated global approach becomes apparent. Stakeholders in the scientific community, bioethics, and policy-making must collaborate to establish set guidelines that prevent misuse and promote responsible use of CRISPR technology.
The Future of CRISPR in Medicine
Looking ahead, the future of CRISPR gene editing technology is both promising and uncertain. Researchers are actively exploring its application not only in curing genetic diseases such as sickle cell but also in combating conditions such as cancer and rare genetic disorders. The continuous advancement in the precision of gene editing tools promises to revolutionize personalized medicine, allowing treatments tailored to individual genetic profiles. However, this potential is accompanied by pressing ethical and safety concerns.
The trajectory of CRISPR technology will significantly depend on how society navigates the ethical dilemmas it presents. Engaging diverse voices in the conversation—from scientists and bioethicists to patients and the public—is essential for developing a well-rounded perspective on gene editing. Future achievements in gene editing must be accompanied by rigorous ethical standards and the commitment to avoiding the pitfalls of inequality, thereby ensuring that the promise of CRISPR can be harnessed for the benefit of all.
Public Perception and Misconceptions About Gene Editing
Public perception plays a critical role in the discourse surrounding CRISPR gene editing technology. Misinformation and misunderstandings about what gene editing entails can shape opinions and influence policy decisions. As such, it is crucial that reliable information reaches the public to foster informed discussions. Awareness campaigns that educate the community about the science of CRISPR, the potential benefits, and the associated risks can aid in demystifying the technology.
Furthermore, the media’s portrayal of gene editing can significantly impact societal attitudes. Responsible journalism is essential in framing CRISPR technology and its applications within an ethical context rather than sensationalizing its capabilities. By promoting transparency and understanding, we can cultivate a public discourse that not only embraces innovation but also critically considers the moral implications, ensuring a balanced approach to the implementation of gene editing technology.
The Role of Bioethics in Gene Editing
Bioethics serves as a guiding framework for the ethical evaluation of advancements like CRISPR gene editing technology. It brings multiple perspectives to the table, integrating moral philosophy, public policy, and scientific research to assess the implications of genetic modifications. As the capabilities of gene editing expand, bioethics will play an essential role in addressing questions of governance, consent, and the potential societal impacts of genetic interventions.
Engaging bioethicists in discussions about CRISPR technology can ensure that ethical considerations remain at the forefront of research and application. This discipline emphasizes the need for dialogue around health equity and access to innovative therapies, highlighting the importance of considering diverse societal values and the potential consequences of modifying human genomes. In this way, bioethics not only contributes to responsible scientific inquiry but also seeks to safeguard the dignity of human life as we navigate the advancements in gene editing.
Conclusion: Balancing Innovation and Ethics in Gene Editing
In conclusion, the dialogue surrounding CRISPR gene editing technology encompasses both remarkable potential and significant ethical challenges. While advancements in gene editing can offer life-changing solutions for individuals suffering from genetic disorders, they also demand careful consideration of equity, consent, and the broader societal impacts. Engaging diverse stakeholders in meaningful discussions ensures that innovation maintains a strong ethical foundation.
As we stand at this crossroads in genetic research, it is our collective responsibility to navigate the ethical landscape with diligence and foresight. Collaboration between scientists, ethicists, and the public is essential to guide the future of gene editing technologies like CRISPR in ways that enhance health equity and promote justice in medical advancements, ultimately allowing us to harness these powerful tools for the greater good.
Frequently Asked Questions
What are the ethical considerations surrounding CRISPR gene editing?
CRISPR gene editing presents several ethical challenges, such as the morality of altering human genetics and the implications of changing traits deemed as ‘normal’ by society. Discussions often focus on whether we should edit genes for diseases like sickle cell anemia or traits like deafness, raising important bioethics issues about autonomy and the role of parents in deciding genetic outcomes for their children.
Can CRISPR gene editing provide a cure for sickle cell disease?
Yes, CRISPR gene editing technology has shown promise in curing sickle cell disease by correcting the genetic mutations responsible for the illness. This manipulation of somatic cells can remove disease-causing genes, offering patients a potential path to recovery and improved health outcomes. However, the high cost of these treatments raises significant health equity concerns.
What are the potential health equity issues related to CRISPR gene editing?
Health equity issues arise from the fact that advanced CRISPR gene editing treatments, such as those for sickle cell disease, can cost millions of dollars. This raises questions about accessibility and the fairness of distribution, particularly for marginalized communities. There is concern that such innovations might widen the gap between those who can afford them and those who cannot.
How does CRISPR gene editing challenge traditional notions of human difference?
CRISPR gene editing challenges our understanding of human variation by raising questions about the desirability of altering traits seen as part of our humanity. For example, ethical dilemmas arise when considering whether traits like deafness should be ‘fixed’ or viewed as simply a form of human diversity. This touches on broader topics in bioethics and the concept of what it means to be human.
What oversight exists regarding the use of CRISPR gene editing technologies?
Although there are legal frameworks restricting certain applications of CRISPR gene editing, such as germline editing, enforcement varies globally. Concerns have been raised about whether countries like Russia or China effectively monitor these practices. This lack of oversight heightens fears of unregulated experimentation and potential misuse of gene editing technologies.
What are the unintended consequences of gene editing with CRISPR technology?
Unintended consequences of CRISPR gene editing may include disruptions to other genetic functions. For example, while editing genes related to cholesterol levels may lower risk for certain diseases, it can also affect other bodily systems due to complex gene interactions that have developed over millions of years. These potential side effects underscore the need for careful ethical consideration and thorough research before broad application.
| Key Points |
|---|
| CRISPR technology has the potential to cure genetic diseases like sickle cell anemia but raises ethical concerns regarding its use and implications. |
| The costs of CRISPR treatments (e.g., $2.2 million for sickle cell) raise questions about access and health equity. |
| Debates exist regarding which conditions are eligible for gene editing, particularly for non-lethal disorders like Down syndrome. |
| The question of parental rights in deciding genetic modifications for children is controversial. |
| There are concerns about global oversight of gene editing practices, particularly in countries with lax regulations. |
| Unintended consequences of gene editing, such as altering genes that impact various biological functions, must be carefully considered. |
Summary
CRISPR gene editing presents groundbreaking opportunities to treat and potentially cure genetic disorders, but it also opens up a myriad of ethical dilemmas. The discussions surrounding CRISPR not only focus on scientific advancements but also challenge us to consider the deeper implications of altering human genetics. As we weigh the benefits against the risks, it becomes clear that responsible practices and ethical considerations must guide this powerful technology to ensure fair access and moral integrity in its application.